Postdoctoral Fellow | Society of Fellows, Dartmouth College
tiina [dot] rosenqvist [at] gmail [dot] com

Research Project #2:
(Chronic) Pain, Credibility,
and Clinical Practice
One key aspect of my research focuses on pain and suffering, with an emphasis on testimonial exchanges surrounding pain.
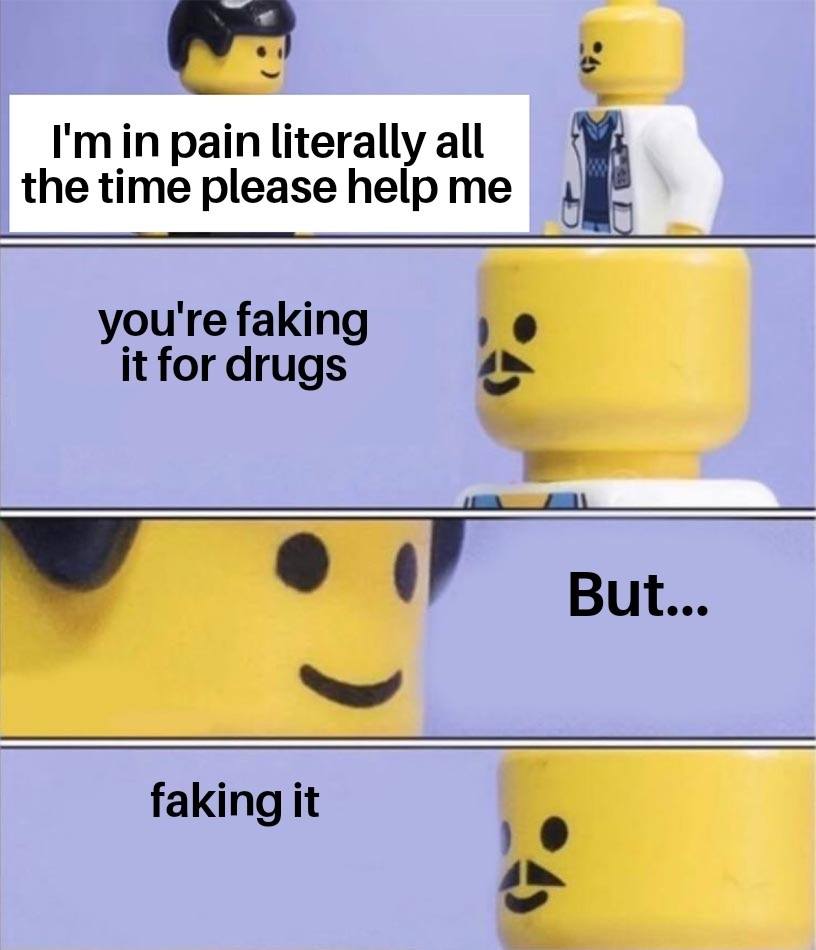
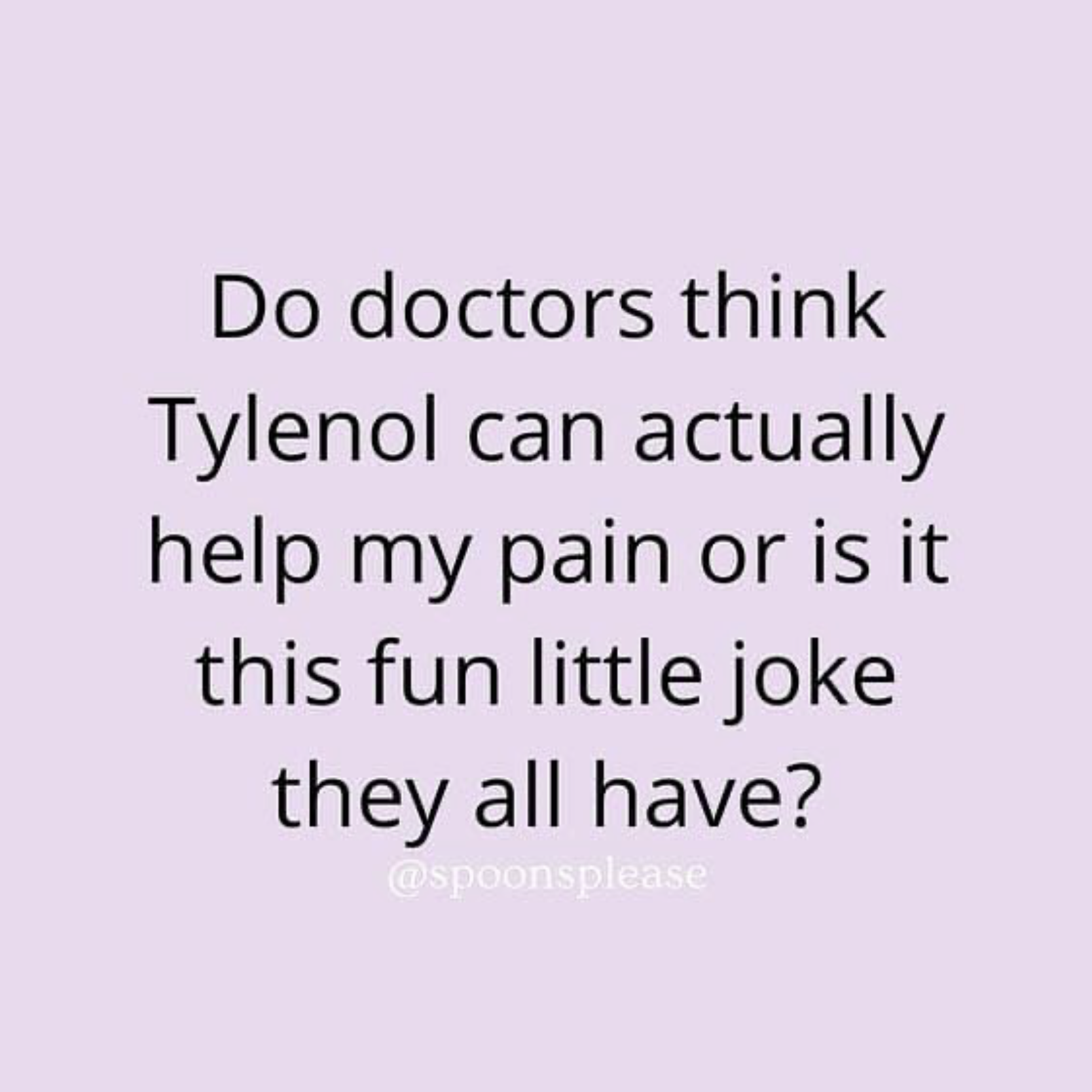
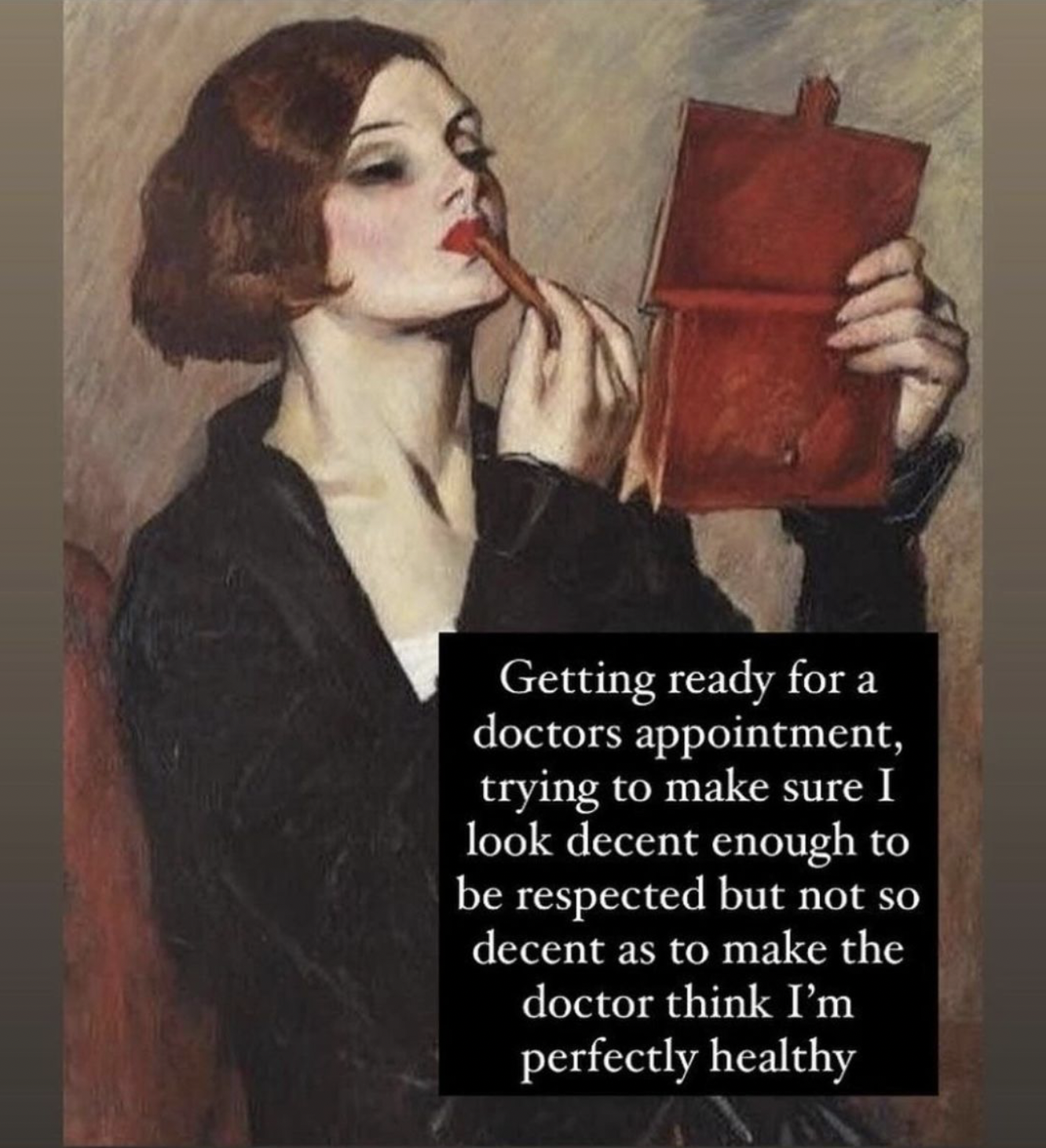
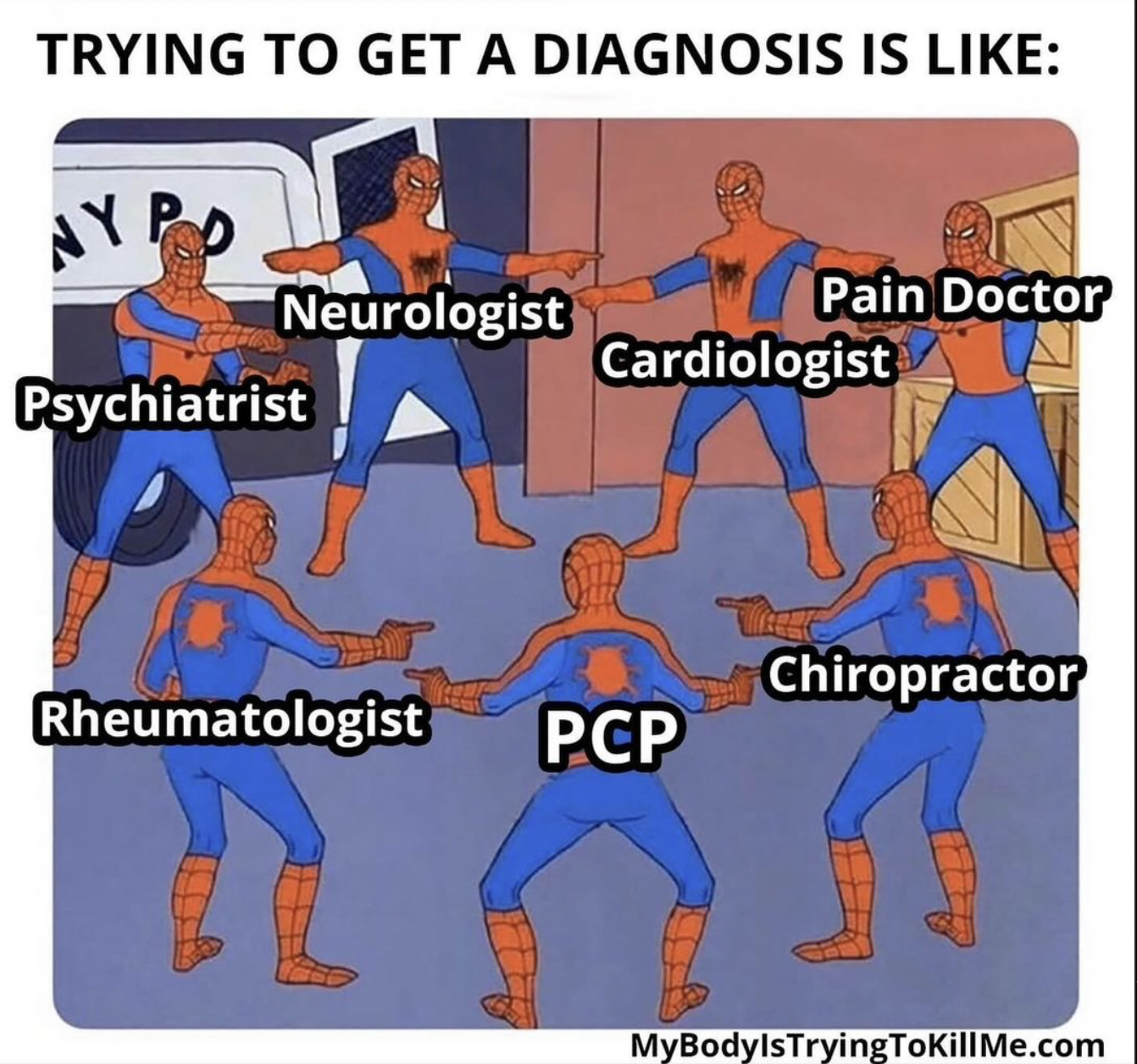
Chronic pain, normally defined as pain lasting for three months or longer, is a public health challenge, a leading cause of disability, and a source of considerable emotional distress for many people. Despite meaningful efforts to reduce the burden of pain and tackle the challenges in its treatment, many chronic pain patients continue to report dissatisfaction with the care they receive. A commonly reported issue is "credibility deficits" in clinical contexts: chronic pain patients often feel that their pain testimony is unfairly doubted or dismissed by doctors and other clinicians.
My goal is to contribute to the improved quality of care for individuals with persistent pain using the tools and methods of philosophy. The project combines philosophy of science, social epistemology, phenomenology, medical ethics, and conceptual engineering to achieve this aim.
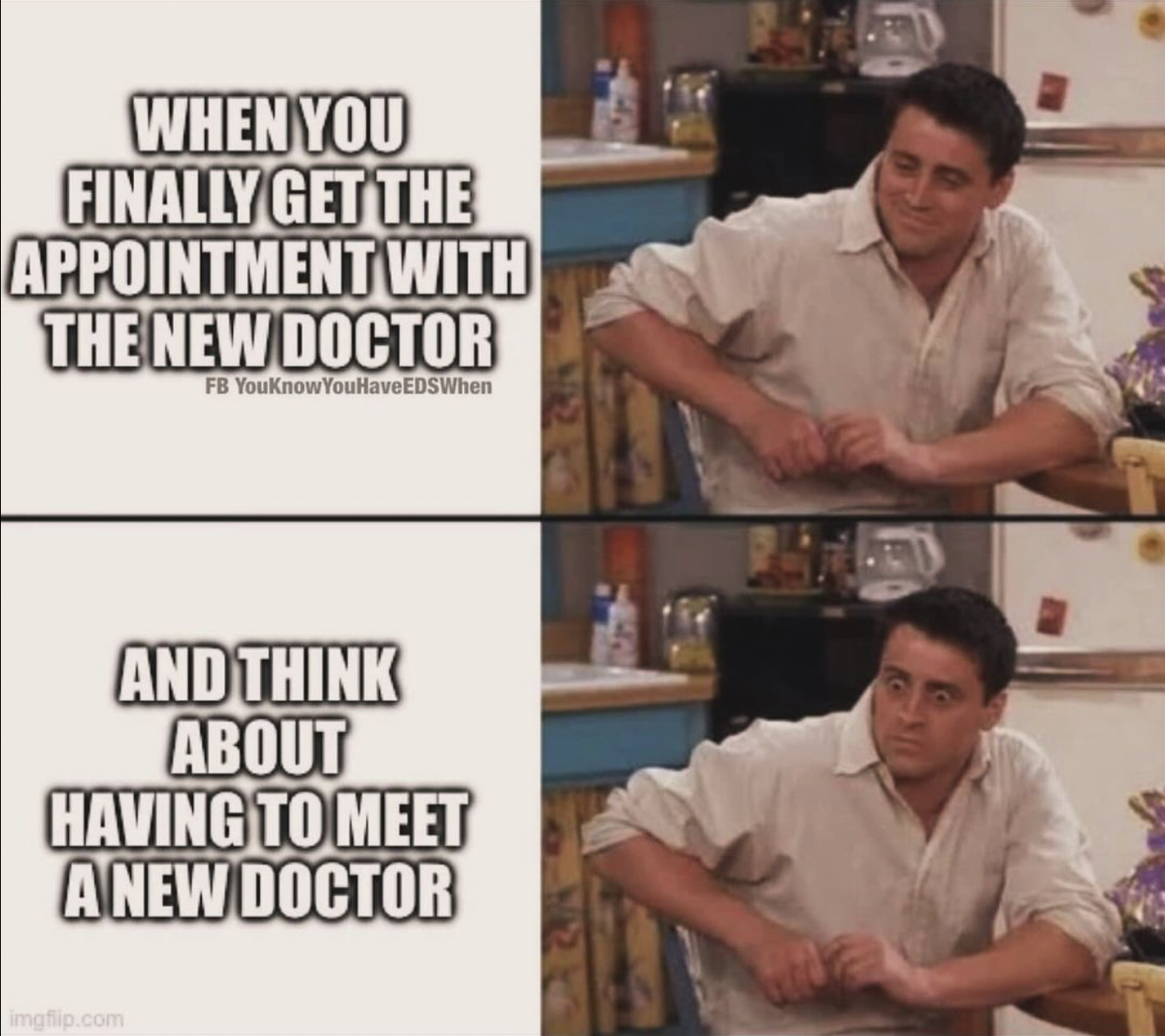
The memes below highlight why this work is necessary: